Flexible Sigmoidoscopy
Examination of the rectum and left side of the colon
What this test involves
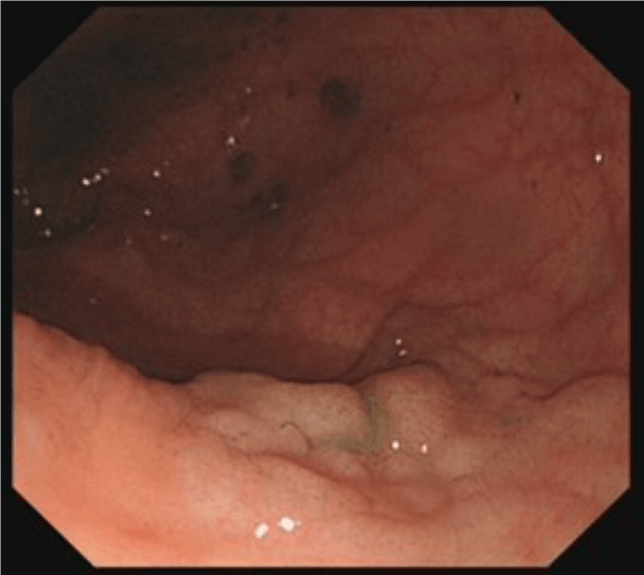
Flexible sigmoidoscopy is a limited form of colonoscopy which involves passing a flexible tube (see image alongside) through the anus into the rectum and steering it around the colon. However, the procedure is limited to looking at the left side of the colon only. The reason for doing this is that certain conditions are more likely to affect only the lower bowel, such as bright red bleeding, or we might wish to check on a site where a polyp was removed. Flexible sigmoidoscopy does not require full bowel preparation and can usually be carried out without sedation or 'gas and air' (Entonox) - however people are quite at liberty to request it if they wish. Although specialised shorter endoscopes exist specifically for flexible sigmoidoscopy, we usually use a colonoscope for this procedure. see images below (hover over the image for a description).
The procedure is not painful but can be uncomfortable due to the gas inserted to distend the bowel and give clear views. We use carbon dioxide to do so which is rapidly absorbed and therefore such bloating does not last for long.
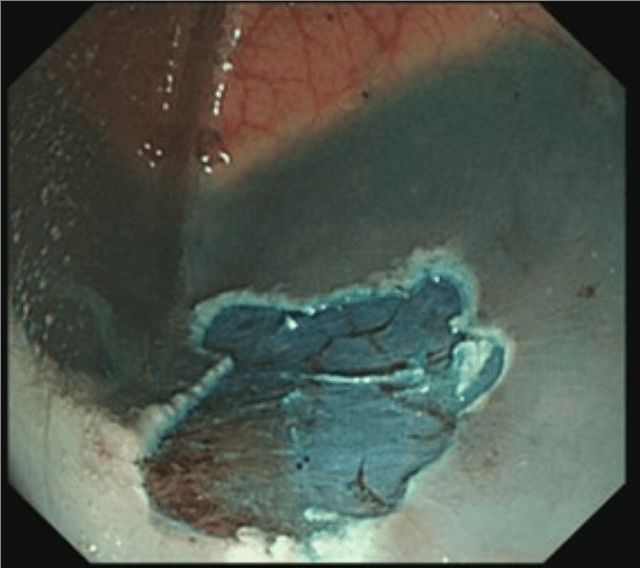
If there are any abnormalities seen, we can introduce instruments down a channel in the sigmoidoscope to take a small sample of the tissue - a 'biopsy'. There are no pain receptors in the lining of the gastrointestinal tract and this is therefore painless. Biopsies are sent off to the laboratory for analysis and usually take 1-2 weeks before we receive a report.
The instrument channel can also be used for treatment purposes - for instance, to remove colonic polyps, or to cauterise bleeding blood vessels.
Risks and safety
Flexible sigmoidoscopy is a very safe procedure and we take every precaution to ensure your well-being and comfort.
Adverse events have been described rarely - in one large study of more than 100,000 individuals undergoing flexible sigmoidoscopy, only 7 experienced significant complications, including 2 episodes of bleeding and 2 perforations.
- Intravenous sedation carries a risk of impaired breathing and inhalation of stomach contents. The sedatives used are short acting and have safe reversal agents. We monitor your oxygen levels and provide additional oxygen throughout the procedure in order to reduce any associated risks of sedation.
- Serious complications include perforation and bleeding:
- Perforation - where the instrument accidentally passes through the wall of the colon. In the above study it occurred in 1:50,000 procedures, but is more common where polyps are removed. It can often be managed by clipping or closing the hole at the time, but may require a stay for observation in hospital and in rare circumstances may require surgery.
- Significant bleeding is very rare and can usually be managed by treating through the endoscope but may require an X-ray procedure or surgery in very rare circumstances.
Instructions and preparation for the test
You will be asked to attend the endoscopy department having administered an enema (provided to you with instructions) to clear our the lower bowel beforehand. if this is not easily possible then we can give you the enema in the department half an hour prior to the procedure taking place. You may eat and drink normally beforehand.
We will discuss the procedure in detail with you on the day and answer any questions you may have, prior to asking for your consent to proceed.
Please make sure that you inform us prior to the procedure about:
- Medications - especially any medications that thin the blood ('anticoagulants') , or for diabetes
- Any severe cardiac or respiratory condition including a pacemaker device.
- Any allergies that you may have to medications (our procedures are latex-free).
After the procedure
You will be taken to a recovery area (if you have had sedation) for us to monitor your blood pressure and oxygen levels whilst the sedation wears off. This can take a few minutes to half an hour or so.
Otherwise you will be given a drink and snack (or meal depending on the unit where you have this procedure undertaken!) before leaving for home.
If you have had sedation, you will need someone to take you home and remain with you as a precaution. We would recommend that you do not use heavy machinery or sign important documents for 24 hours after the procedure.
I will inform you of the findings of the test and if any biopsies have been taken that mean we have to wait for additional results from the laboratory. You will be provided with a copy of your report (usually with photographs for your records).
If you experience any significant symptoms within the following 48 hours after the test - including pain, fever, vomiting blood or passing black bowel motions then please contact the unit immediately for further advice - they will put you in touch with me.